A brief look at the history of public health from Antiquity to now.
Innovative Approaches to Pandemic Response
How Do Pandemics End?
mRNA Vaccines
COVID FAQs: Vaccine
COVID FAQs: Variants
We compiled some of the most common questions about the COVID-19 variants.
This article was written February 18th, 2021 and reflects the science as of that day.
Why are there variants of COVID-19?
Viruses mutate frequently. Most of the time, the mutations are harmless and have no effect on the virus at all. However, once in a while a mutation is able to amplify some characteristic. In our case, the new variants are able to spread more efficiently from person to person. As time goes on, this may become the dominant strain of the virus due to its improvement. This is evolution/natural selection/survival of the fittest happening in real time.
What are the characteristics of the variant?
The major change in the UK and South African variants is that they are more easily transmissible between people. The South African and Brazilian variants have also seemed to change the way our antibodies are able to bind to them but further research is needed to assess the differences.
Do the mRNA vaccines still work against the variant?
Early studies say yes! The vaccines are still effective against the variants however the immune response may not be as strong or prolonged.
If I’ve had COVID-19 already, should I be worried about getting the new variant still?
The reinfection possibility is still being studied, however recent research has shown that antibodies produced during infection only last up to 5 months. Even if you’ve had COVID-19 you should still take precautions to prevent infection from both variants.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
Vaccines 101
Transportation Strategies
Planes
Air travel was almost nonexistent at the beginning of the pandemic. Flights were far and few between but now the industry has adapted with safety and sanitation precautions to keep employees and travelers healthy. However, there are still risks associated with air travel.
If you do choose to travel via airplane, make sure the airline requires passengers to wear masks. It is difficult for pathogens to spread in airplanes because of how air circulates and filters in a pressurized cabin but the mask will help even more.
Make sure to distance yourself from other passengers. This can be difficult on a crowded flight but most airlines are limiting capacity of planes and keeping middle seats empty. You can also strategically book your flights to avoid contact with large crowds. Some airlines allow you to choose your seats before booking and you can gauge how many people will be on the flight. Flights on weekdays are usually less crowded than weekend flights.
Follow the same rules you’ve been sticking to since the pandemic hit. Social distance, wear a mask, and wash your hands thoroughly and often.
Trains and other forms of public transport
Public transport is probably the most difficult method of transport to navigate during the pandemic. While most transit systems are limiting capacity, it can be difficult to feel safe in small crowded spaces. Keep up to date on rules and requirements made by local transit authorities to decide if it is a good idea to use it.
If you do choose to use public transit, follow the same rules you’ve been sticking to since the pandemic hit. Social distance, wear a mask, and wash your hands thoroughly and often.
Automobiles
If you’re in a rideshare/taxi it is very important that everyone is wearing a mask and that the windows are open if they can be. Even with a plastic divider between passengers and drivers, you are not sealed off from each other in any way.
Road trips aren’t without their share of risk either. Breaks at gas stations, rest stops, and anywhere along the way carries potential exposure to COVID, especially in high case areas.
If you do choose to take a rideshare/taxi or go on a road trip, follow the same rules you’ve been sticking to since the pandemic hit. Social distance, wear a mask, and wash your hands thoroughly and often.
Even if you don’t end up traveling during the pandemic, social distance, wear a mask and wash your hands thoroughly and often.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
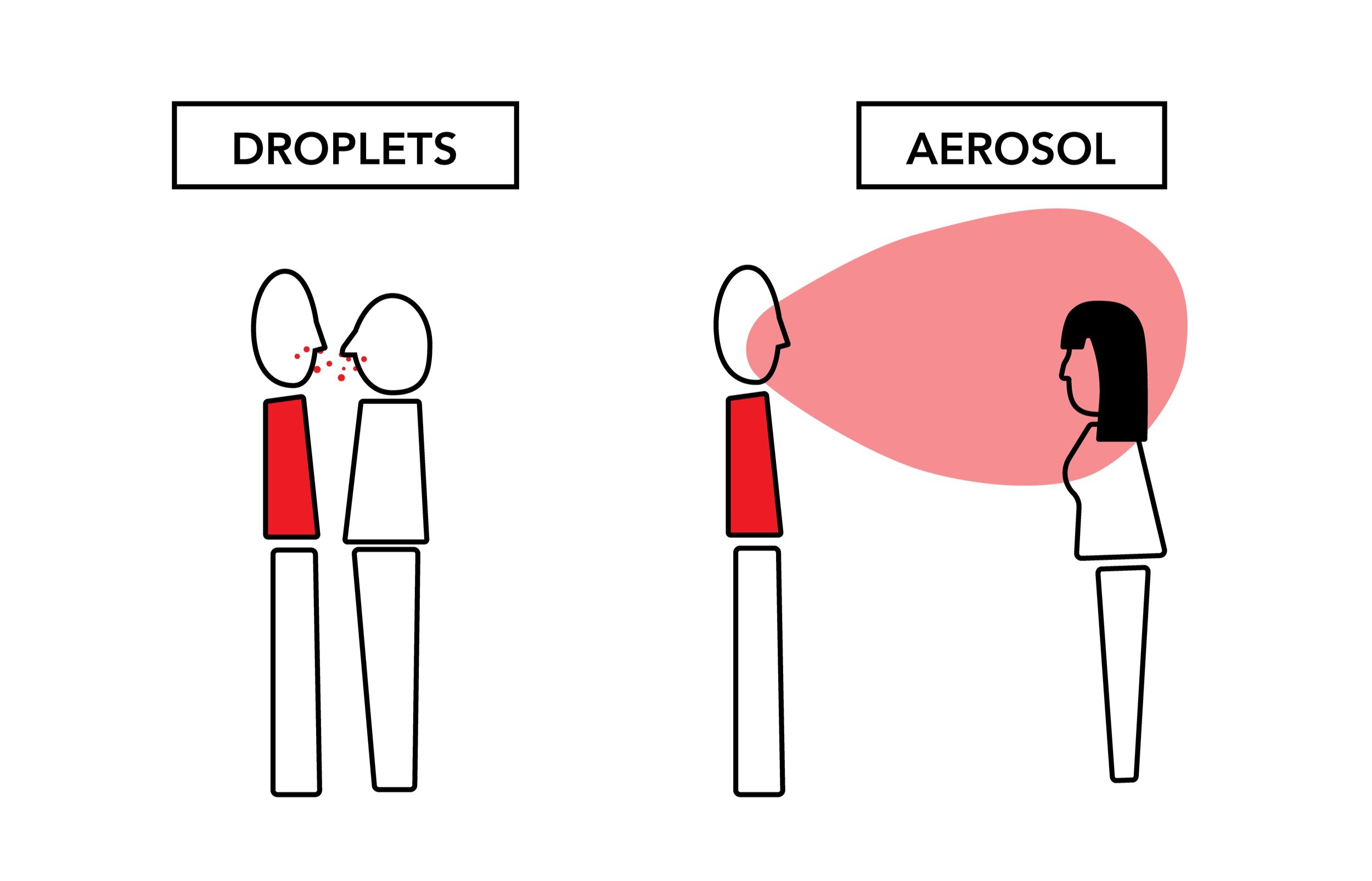
Aerosols Pt. 2
COVID-19 has proven to be an incredible infectious disease. It is able to spread in two major ways: through droplets caused by actions like coughing and then aerosols that occur while we speak and breathe. By limiting the exposure of droplets and air contaminated with the virus we can thus limit infection. Precautions such as wearing a mask, staying at least 6 feet away from other people, and limiting social gatherings to outdoor spaces all help. However, many people that gather outdoors fail to wear a mask or socially distance themselves because they think that being outdoors is enough. This is not true.
Although the risk of contracting COVID through outdoor activities is about 20 times less than indoors, the risk is still there. Modeling droplet and aerosol transmission outdoors is a lot more difficult than modeling indoor interactions due to the amount of variables to take account for. It is still important to take the proper precautions while outside to decrease the risk of transmission.
One of the most important outdoor variables that decreases transmission risk is humidity. Studies have shown that high humidity correlates to lower concentrations of aerosolized pathogens and increases the clearance of pathogens in mucus membranes (nose and throat). This leads to less risk of transmission of disease by aerosols and droplets. On the other side, low humidity increases the risk of transmission and is a main driver of cold/flu season in the late fall and winter months. While gathering outdoors, we want to have the lowest risk of transmission of COVID and other diseases. It is impossible to eliminate risk without choosing not to gather at all. To decrease the risk as much we can, it is so important to continue to socially distance and wear a mask.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
Personal Strategies
We've published many different infographics over the last fews months outlining the different actions you can take to slow the spread of the virus and protect yourself and others. Here's a compilation of the key ideas:
Wear a Mask
Not all masks are created equal. If available, always try to get a K/N95 or surgical mask. Make sure to wear it properly (covering nose and mouth), dispose of or clean frequently, and still distance when wearing one.
K/N95 - The gold standard, filters 95% of SARS-COV-2. Can be disinfected after wearing for reuse.
Surgical - 2nd place, filters 95% of SARS-COV-2. Single-use only.
Cloth masks - Make sure these masks are made of safe and breathable materials. Models have shown that multiple layers of a cotton blend offer the best balance of filtration and breathability.
Face shields - Should only be used in combination with effective masks. Alone they do nothing.
Bandanas, scarves, gaiters, fleece, etc. - Not effective and some materials can actually exacerbate aerosol spread.
Learn more about masks here.
Wash Your Hands
While it’s mostly aerosol based transmission with COVID-19, you still need to take precautions with surfaces. Washing your hands with clean running water and soap can remove 99.99% of germs, including COVID-19, from your hands. Because of how easy and effective handwashing is, there is a significant investment in handwashing promotional materials demonstrating effective practices.
Get a Flu Vaccine
Getting your flu shot not only protects yourself but everyone around you. It also keeps you out of medical offices where there are other sick patients. By keeping the flu cases down, we can help ease the strain on the medical infrastructure that is being overwhelmed by COVID patients. We can keep hospital beds, medical personnel, and vital supplies open to other patients. Learn more here.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
How Pandemics Happen: Pt. 1
Masks 101
There are so many different masks available for purchase now. When the pandemic started, there was a shortage and most people just used what they could get their hands on. Homemade cloth masks were worn by most, while surgical masks and the gold standard N95 were reserved for front-line workers and essential personnel. Now that all kinds of masks are available, what are the differences between them?
N95 / KN95
These masks are rated for their ability to filter particles that are 0.3 microns in diameter. The 95 signifies that they are able to filter 95% of these particles. There are also 99 and 100 masks but they are not widely available for consumers. They are rated at filtering this size because of their intended use, non-biological safety. However due to the material they are made of, these masks are able to filter particles less than 0.1 microns in diameter (SARS-COV-2 is reported as 0.12 microns). These masks are the most effective widely produced masks and reusable. To clean them at home just spray them thoroughly with rubbing alcohol or hydrogen peroxide and let them air dry for at least 24 hours. There are also procedures where the mask is placed in an oven set on a low temperature, however this may damage the mask straps if they are attached by adhesives.
Surgical Masks
Most surgical masks that are found in stores are rated at US Level 1 meaning they filter 95% of 3.0 micron diameter particles and 95% of 0.1 micron particles. Surgical masks are rated at smaller filtration sizes because they are used in biological settings where bacteria and viruses are present. These masks are available to purchase in large packs but it is important to only use each mask once. They cannot be cleaned like N95 or cloth masks because of the type of plastic used to make them.
Cloth Masks
If N95 or surgical masks are unavailable to you, cloth masks can be used as a substitute. When searching for cloth masks, there is a balance between breathability and efficiency. If making your own, the best material for both is actually high thread count antimicrobial pillow cases. A single layer of a pillowcase offers 60% filtration against 0.02-micron particles, much smaller than the SARS-COV-2 virus. If purchasing cotton masks, look for masks that are made of multiple layers of a cotton blend. Both of these cloth masks can be washed either by hand or in a washing machine with detergent or soap and dried in a machine or in the air depending on the strap. If the straps are glued on, make sure not to expose them to too much heat.
Bandanas/Gaiters/Scarves
Not effective at air filtration for users and people around you. Certain materials, most notably fleece, actually helps create more droplets and increase the spread of pathogens in the air.
Face shields
Not effective at shielding against airborne pathogens.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
COVID 101: Infographic Collection
Get a Flu Vaccination
Why the Flu Vaccination Protects Everyone
Getting your flu vaccine is particularly important this year. Although the flu vaccine does not make you immune to COVID-19, it does significantly decrease your chances of being exposed in healthcare settings. It is important to note that the influenza virus causes the flu and SARS-COV-2 causes COVID-19. The flu shot lessens the likelihood of getting the flu which protects you from getting both the flu and COVID which would be dangerous.
With the predicted third wave of COVID-19 cases hitting the United States (and most of the world) during the late fall and early winter months of 2020, hospitals and healthcare facilities are being overwhelmed by COVID patients. As of early December in the US, there are nearly 100,000 people currently hospitalized due to severe COVID symptoms and inching towards 15 million cumulative infections.
Over the course of the 2019-2020 flu season, the CDC estimates that there were 17 million medical visits, 500 thousand hospitalizations, and 34 thousand deaths attributable to the flu in the United States. Although estimates for the 2020-2021 season so far are much lower than previous years due to social distancing measures and people wearing masks, it is important to mitigate the risk as much as possible. If more people get the vaccine, less will be seriously hospitalized with the flu which will open up hospital beds and capacity.
By getting the flu shot, you’re not only protecting yourself. You are also protecting those around you like the elderly, people who have allergies to vaccines, and arguably most importantly, medical caregivers. This will lighten hospital personnel’s workload and allow for a higher level of care capacity. The flu vaccine is typically anywhere between 40 and 60% effective most years, combined with social distancing and wearing masks this year, the burden of the flu can be significantly reduced from previous years.
Find where to get a flu vaccine near you:
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Navigating the Holidays
With the holiday season quickly approaching, visiting families and friends is going to be very different due the COVID-19 pandemic. Limiting exposure to family members, especially our elders, is going to have to be kept in mind for safe visitations. Video chatting is the best option, but we have some risk mitigation ideas if your gathering must be in person. It’s our responsibility to protect each other and help end the pandemic.
Video chatting is the safest way to see family and friends because there’s no exposure! There are plenty of platforms out there. Get creative. Try learning new cooking techniques on video with friends. Include family members who aren’t normally able to make it in person. Treat it as an opportunity, not a waste.
Make sure to quarantine for at least 2 weeks before visiting people or being exposed to anyone outside of your bubble.
Get a COVID virus test before you travel and upon arrival. Be aware that a negative test doesn’t mean you’re fully safe from developing COVID or infecting others depending on when you test. Make sure to follow all testing guidelines and wear a mask to and from the facility.
Remember the basics: Wear a mask when with anyone not in your bubble (outside or inside), keep at least 6 feet of space between people, and wash your hands thoroughly and often.
The best setting for a visit is outdoors - with masks still. Try opening up the garage or adding space heaters to a patio. If you have to be indoors, take the steps to ensure proper ventilation, filtration, and humidity in indoor spaces
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
COVID & Ultraviolet
SARS-CoV-2 in the Air
COVID-19, Wildfires, Air, and You
This Testing Stuff is Confusing!
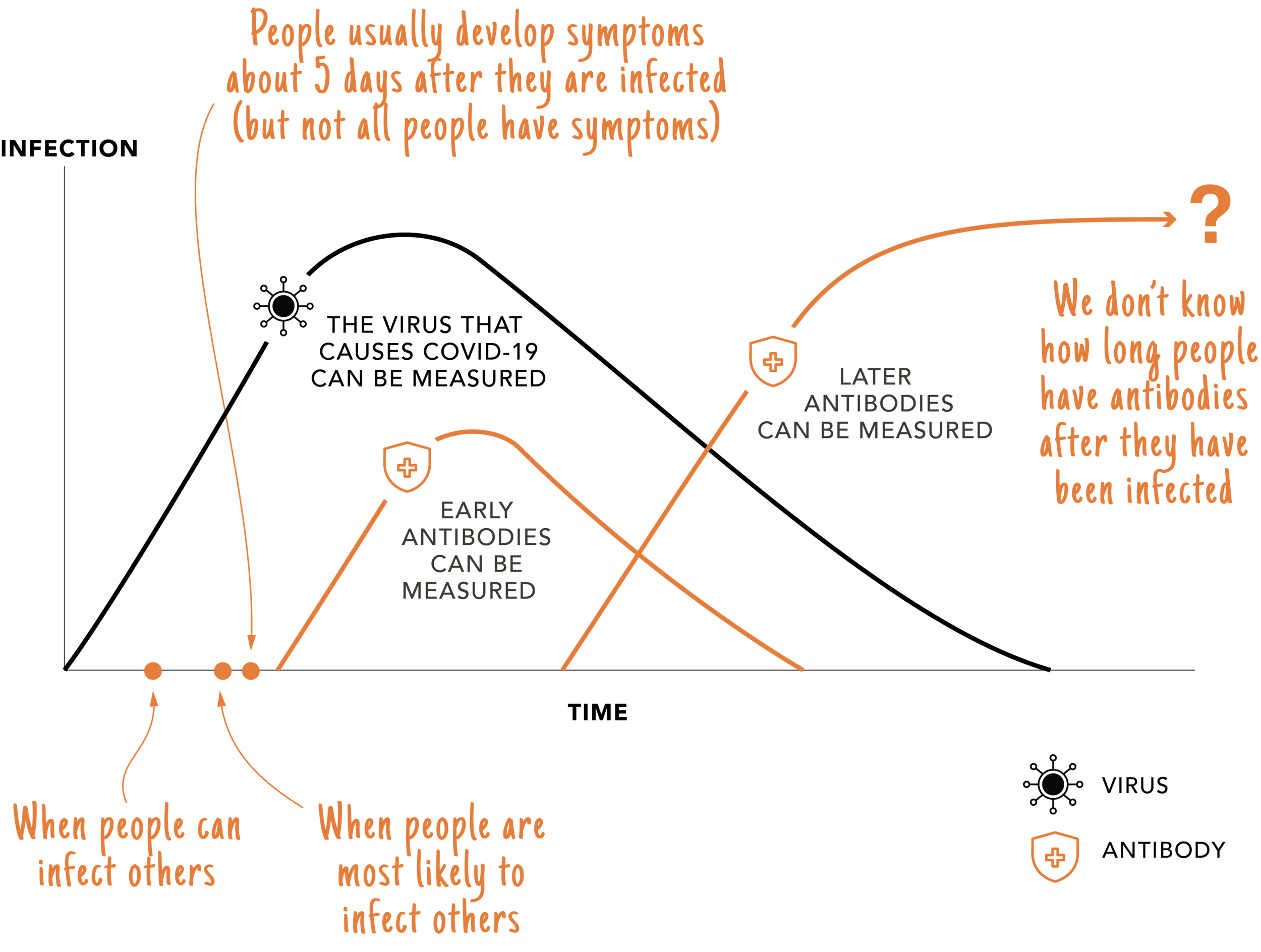
Some COVID-19 tests look for the virus (SARS-CoV-2) that causes COVID-19 and some tests measure antibodies our body creates to fight the virus. The black line below shows the virus during infection and the orange lines shows two types of antibodies that our body creates after we have been infected. This chart illustrates how SARS-CoV-2 (Virus) and antibody testing related to each other and is based on what is known as of May 2020.
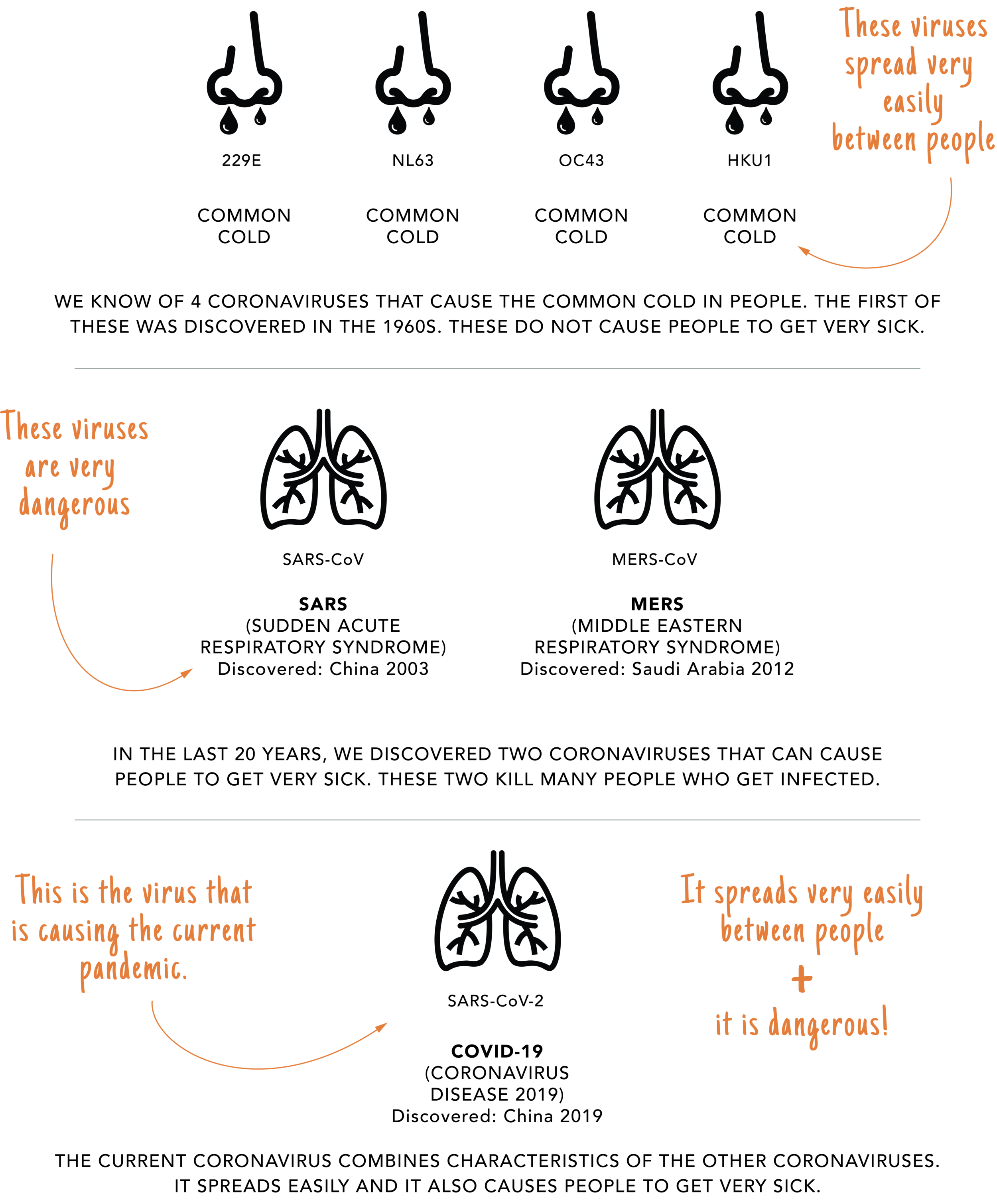
What Do We Know About Coronaviruses?
There are 7 coronaviruses that we know cause illness in people. Four of them cause upper respiratory illnesses (a.k.a., common colds). Three of them are lower respiratory illnesses and have been discovered in the last 20 years. These coronaviruses are more serious.